
We attended a local meeting in Anzola dell'Emilia, a municipality in the hinterland of Bologna, which saw the participation ofRegional Councilor Raffaele Donini, also coordinator of the Health Commission of the Conference of Regions, and of the General manager of the Paolo Bordon Health Authority of Bologna. Interesting to better understand how the new territorial assistance reform is being worked on, which with the DM77 has become state law. A reform that promises to change the face of our country's healthcare, trying to imagine how it will be able to graft itself into a fabric of daily problems and extraordinary peculiarities.
First of all, in addition to greetings and thanks, the Mayor Giampiero Veronesi reveals that the project of the Community House of Anzola, financed by the PNRR, will receive an additional investment from the Municipality, which wants it to be even more responsive to the needs of citizens.
Even in the thriving and organized Emilia Romagna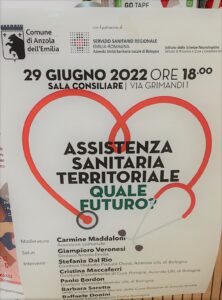 the problems are not lacking according to the Dr. Cristina Maccaferri, Director of Primary Care of the District, “We are in a moment of great transformation. The pandemic has changed the way we work, the relationship with patients, the way we communicate."
the problems are not lacking according to the Dr. Cristina Maccaferri, Director of Primary Care of the District, “We are in a moment of great transformation. The pandemic has changed the way we work, the relationship with patients, the way we communicate."
In fact, we must not forget that we are thinking about the future of healthcare in the midst of a health emergency that is not marking time. “I can testify to the great difficulties we had to face during the pandemic period – says la Dr. Barbara Saretta, family doctor and manager of a group of 7 doctors – A colleague of the group retired slightly early, but at a time of great commitment. So we huddled together and coped. We have agreed to be present H12 and Saturday and Sunday by telephone. But there has never been a break and even today there are a huge number of patients, which is why we had to limit access to the clinic again" "We want to not get sick: if 5 of our group get sick, what would happen?”
Find new general practitioners that they are ready to settle is not easy and the problem arises of making themselves more "attractive". Shortage of medical personnel is a global problem  and it does not only concern primary care, but all specialties throughout the national territory. With few doctors and many areas available, one of the characteristics considered preferential is the offer of an outpatient clinic within the local health facilities. This territory can actually boast some very advanced conditions: the presence of numerous group medicines, recognized as a very important element during the pandemic, in addition to the fact that these are often organized with the study assistant and the secretary. Not only that, but the Houses of Health they are already widespread in Emilia Romagna which counts 130 out of about 500 present throughout the country.
and it does not only concern primary care, but all specialties throughout the national territory. With few doctors and many areas available, one of the characteristics considered preferential is the offer of an outpatient clinic within the local health facilities. This territory can actually boast some very advanced conditions: the presence of numerous group medicines, recognized as a very important element during the pandemic, in addition to the fact that these are often organized with the study assistant and the secretary. Not only that, but the Houses of Health they are already widespread in Emilia Romagna which counts 130 out of about 500 present throughout the country.
“The PNRR envisages investments primarily in Community Houses, which are the evolution of the Casa della Salute” – he says Paolo Bordon, General Manager of the Company – but with a strong integration between the health and social services, plus the voluntary associations, which work alongside the health workers and are in fact part of the system" "The challenge being launched is that of a partnership between public subjects to manage the proximity of care. Bring health services, integrated with social services, as close as possible to the patient. The home can be the first place of care, investing more and more in territorial functions”
The management of chronicity it is therefore one of the axes of the reform. “From the Community House we will also be able to use advanced tools such as the telemedicine, giving the possibility for professionals to deal with second-level specialists, and other figures are also envisaged such asFamily Nurse, which will be the first interface for the general practitioner in taking charge of the chronic patient, and theCommunity nurse, which will work at a higher level and with a wider pool, to allow easier integration between all subjects and social services."
possibility for professionals to deal with second-level specialists, and other figures are also envisaged such asFamily Nurse, which will be the first interface for the general practitioner in taking charge of the chronic patient, and theCommunity nurse, which will work at a higher level and with a wider pool, to allow easier integration between all subjects and social services."
It's time forCouncilor Raffaele Donini: “Today we find ourselves thinking about the project for the future of health care for the next 20 or 30 years in the paradoxical situation of still being in full emergency. The reforms we are preparing and which are already state law represent the prospect, the fruits that will be reaped in 3-5 years. But today we cannot divide, we must create a system, reject partisan exploitation and study bridging solutions. The themes are mainly three: General Medicine, Emergency Department, Hospitals and some departments in particular.
“The shortage of healthcare personnel, even for those who represent excellence, heavily affects the present. In the face of retirement and burnout we can't replace doctors. The shortage of doctors and health personnel is a national problem and the result of 20 years of cuts to the health system.”
In the face of retirement and burnout we can't replace doctors. The shortage of doctors and health personnel is a national problem and the result of 20 years of cuts to the health system.”
“Doctors, as represented here in Anzola, who work together, collaborate and help each other are an example at a national level. We could talk about multidisciplinarity also among GPs, each with its second specialty, its background, its experience. Comparison improves diagnostic ability and raises the level of care.” "When a so-called organ specialist and someone who knows the patient's clinical history meet (think of telemedicine) the maximum performance we can produce is achieved."
The General Medicine
"After setting aside the prospect of a dependency relationship for the MMG - Councilor Donini continues - after the earthquake that the proposal has unleashed, How do we get through the bridging period? First we must increase the ceiling bringing it, as a proposal, to 1800 patients. Then, making use of a state law, we can envisage doctors in the 2nd or 3rd year of the training course for general medicine, to take care of an average of 1,000 patients. Alternatively or alongside this we can think of fielding continuity of care clinics, community doctors, but they are not GPs, with all that follows.”
“Since, however many resources are made available to train new professionals, we must ask doctors to make an effort to face this transition period already exhausted, what can we make available to allow them to work at their best? We are thinking about funding or structures for the administrative secretariat. Also to a nursing network, as someone has already organized, at their disposal to reach the patient's home. So we're doing our best and we'll find a solution because the alternative, which nobody wants, would be to leave citizens without a general practitioner."
“The reform of the relationship with general medicine is ready, has the consent of the Fimmg, the Ministry of Health, the Health Commission of the Regions, so I think that by the summer it could be presented by the Government. There is the problem of distributing the hours that doctors should work in the structures, 18 a week, making them compatible with the large loads that the emergency imposes, but we are confident in a near solution."
The Emergency Departments
“We made a wonderful agreement on the emergency departments, with all the trade union representatives, to remedy in the first place the escape from the emergency and urgency. Faced with exhausting shifts, a strenuous job and the incompatibility with the free profession, very few young people choose this difficult area.  So we looked for solutions to make Emergency Departments more attractive, offering more career opportunities, recognizing, with the formula of additional work instead of overtime, a practically double salary, agreeing investments in more advanced performing instruments, and above all trying to create routes to remove patients recognized in white code from the Emergency Department, the 75% of accesses. As? One solution could be that of outpatient clinics, with continuity of care doctors, who collect the white codes from the triage, currently inside the Emergency Departments themselves, when we will be ready in the community homes."
So we looked for solutions to make Emergency Departments more attractive, offering more career opportunities, recognizing, with the formula of additional work instead of overtime, a practically double salary, agreeing investments in more advanced performing instruments, and above all trying to create routes to remove patients recognized in white code from the Emergency Department, the 75% of accesses. As? One solution could be that of outpatient clinics, with continuity of care doctors, who collect the white codes from the triage, currently inside the Emergency Departments themselves, when we will be ready in the community homes."
“Finally the financial issue. Those who want to provide good health care need three things: funding, because health care costs a lot, personnel (and we have already said this), and good planning, since innovation can also be incorporated into good planning .”
“Our Region, – concludes Donini – which up to now has always been perfect, has been constantly in deficit since 2020. Covid drained hundreds of millions from the coffers of the regions, the management was that of the Extraordinary Commissioner, and the regions have not yet received reimbursement. We do not want either a new centralization or a push towards privatisation. We want to re-appropriate what we do well.”
Editor's note:
- On the Community hospitals, the so-called spokes, only a few brief remarks were made but, as mentioned, the theme of hospitals is essential. It is difficult to think of a serious reform of territorial assistance that does not connect perfectly with an equally careful organization of the hospital network. (you see Forum of hospital clinicians – Prof. Cognetti)
- To the analysis of the problems of the Emergency Department, common to many countries, a large literature is dedicated (1) and the relevance from the point of view of the results of a prolonged stay in the wards is also highlighted. It therefore seems difficult for us to remedy this serious situation, defined by some as the funnel of health care, regardless of interventions upstream of the emergency room, reducing the influx and appropriateness, inside the emergency room, carefully selecting the problems and directing patients in the most suitable and fluid path, e downstream of the emergency room, ensuring an adequate flow towards the hospitalization wards for those patients requiring hospitalization (estimated between 15 and 20% of admissions).(2)
- The debate on the subject of DM 77 inflames the hearts of insiders as much as it goes unnoticed in the "secular" press. We report the presentation by Dr. Domenico Mantoan, General Manager of AGENAS, the company in charge of monitoring the plan, and a document from the trade union federations (cgil, cisl) for a law of retaliation.
(1) – Matthew Cooke et al (editors). Reducing Attendances and Waits in Emergency Departments. A systematic review of present innovations [PDF: 550Kb]. Report to the National Co-ordinating Center for NHS Service Delivery and Organization R & D (NCCSDO) – 2005.





