III Report, few funds, too many benefits in the Lea, waste and insurance expansion
Posted on: 05/06/2018 – adnkronos
"Progressive definancing, too many benefits in the new Lea, waste and inefficiency, expansion of insurance intermediation represent a lethal mixture for public health". Faced with this situation, the new government is facing “a crossroads: relaunch or dismantle the NHS?“. To take stock of the state of health of the National Health Service is the Gimbe Foundation with the third Report on the sustainability of the NHS, presented today in the Chapter House of the Senate in Rome.
The data, especially those on expenditure and the definancing of the system, do not bode well. "We reiterate that there is no hidden plan for the dismantling and privatization of the National Health Service, but a precise rescue plan continues to be lacking - underlines the president of the Foundation, Nino Cartabellotta – In the awareness that healthcare represents both a considerable chapter of public expenditure to be optimized and a lever of economic development to be supported, the Report assesses with
 a medium-term perspective the issue of sustainability of the NHS, starting from its primary objective: to promote, maintain and recover people's health".
a medium-term perspective the issue of sustainability of the NHS, starting from its primary objective: to promote, maintain and recover people's health".
The substantial analysis opens with the results of a systematic review of the international rankings evaluating the performance of health systems. "We need to stop the exploitation in the public debate and in institutional communications - Cartabellotta points out - which praise the prestigious positions of our NHS in now obsolete rankings (second place in the 2000 WHO ranking, with 1997 data), or which relate life expectancy to per capita health spending (third place in the Bloomberg ranking) so the less we spend the more we climb the rankings, given that longevity depends above all on other reasons". It is true, however, that spending on public health continues to fall.
According to the report, the healthcare expenditure in 2016 it amounted to 157.613 billion euros, of which 112.182 billion in public expenditure; 45.431 billion of private spending, of which 5.601 billion of intermediary (3.831 billion from health funds, 593 million from individual policies, 1.177 billion from other entities) and a good 39.830 billion paid by families. "Beyond re-evaluating absolute figures and the percentage composition of health spending - explains Cartabellotta - the real challenge is to identify the return in terms of health of the resources invested: our preliminary estimates show that 19% of public spending, at least 40% of out-of-pocket spending and 50% of intermediated spending do not produce any return in terms of health", highlights the expert.
In the period 2013-2018, compared to almost 7 billion euro of nominal increase in funding, less than 6 billion 'survived'. And in the years 2015-2018, the implementation of public finance objectives subtracted 12.11 billion euros from the planned levels. “With such progressive definancing – underlines Cartabellotta – Italy continues inexorably to lose ground in comparison with other countries, with a percentage of GDP and per capita expenditure lower than the OECD average and which are getting closer and closer to Eastern European countries”. No light - according to Gimbe - can be seen at the end of the tunnel since the Def 2018against an expected annual growth of nominal GDP of 3% in the three-year period 2018-2020, it reduces the health expenditure/GDP ratio from 6.6% in 2018 to 6.4% in 2019, to 6.3% in 2020 and 2021. pathologies", such as definancing, "which risk compromising the prognosis".
They amount to over 21 billion of euros the resources for health care 'burnt' in waste, inefficiency and fraud in 2017. In fact, the report updates the estimates on the impact of waste on public healthcare spending in 2017, as much as 21.59 billion euros eroded by over-use of ineffective or inappropriate healthcare services and benefits (6.48 billion), fraud and abuse (4.75 billion), excessive cost purchases (2.16 billion), under-use of effective and appropriate services and benefits (3.24 billion), administrative complexities (2.37 billion), inadequate coordination of assistance (2 .59 billion). The good news is that, compared to 2016 estimates, more than 1.3 billion euros have been recovered, thanks to the numerous interventions implemented, the Foundation points out.
According to the Report, various criticalities are found in the chapter Leahthe essential levels of assistance. For Cartabellotta, "in the impossibility of increasing public funding, it is essential to reassess all the services included in the Lea in order to implement a 'substantial reduction' and put an end to the unacceptable paradox whereby in Italy the richest 'Lea basket' (on paper) and one of the lowest public funding in Europe coexist".
In this framework, the 'second pillar', the integrative healthcare. “The proposal to rely on the 'second  pillar' to guarantee the sustainability of the NHS - explains the president - has gradually established itself due to the interaction of various factors: in particular, in the cracks of a fragmented and incomplete legislation that has allowed supplementary healthcare to become a substitute, a refined marketing strategy has crept in, fueled by catastrophic, but far-fetched, results on the renunciation of treatment". The Report analyzes in detail the complex ecosystem of 'third-party payers' in healthcare, the coverage offered, the impact of healthcare funds and insurance policies on healthcare expenditure and also the potential side effects: from sustainability risks to privatization risks, from the increase in inequalities to the increase in healthcare spending, from the over-use of healthcare services to the fragmentation of healthcare pathways.
pillar' to guarantee the sustainability of the NHS - explains the president - has gradually established itself due to the interaction of various factors: in particular, in the cracks of a fragmented and incomplete legislation that has allowed supplementary healthcare to become a substitute, a refined marketing strategy has crept in, fueled by catastrophic, but far-fetched, results on the renunciation of treatment". The Report analyzes in detail the complex ecosystem of 'third-party payers' in healthcare, the coverage offered, the impact of healthcare funds and insurance policies on healthcare expenditure and also the potential side effects: from sustainability risks to privatization risks, from the increase in inequalities to the increase in healthcare spending, from the over-use of healthcare services to the fragmentation of healthcare pathways.
Here, then, the prognosis. By 2025, according to estimates in the Gimbe Report, the NHS requirement will be 220 billion. With an estimated increase in total health expenditure in the period 2017-2025 of 27 billion (9 billion of public spending and 18 billion of private expenditure) it would reach just over 184 billion in 2025. To these would be added about 15 billion from the gradual recovery of resources from waste and inefficiency. And yet, Cartabellotta intervenes, "20.5 billion would still be missing to reach the estimated requirement, a figure that requires precise political choices".
In other words, "since the solution is certainly not represented by the 'second pillar', without a substantial relaunch of public funding it will be impossible to maintain a fair and universal public health service - he concludes - Given that the actions of the next executive will be crucial for the future of the NHS, Gimbe will monitor the government health program because the right to protect the health of Italians is today more than ever conditioned by political choices. If one really intends to preserve the greatest conquest of Italian citizens, in addition to increasing the return in terms of health of the money invested in healthcare, it is essential to reverse the trend on public funding".
On 5 June 2018, the GIMBE Foundation presented the 3rd Report on the sustainability of the National Health Service, reiterating that there is no hidden plan for the dismantling and privatization of the National Health Service, but a precise rescue plan continues to be lacking.
In the awareness that healthcare represents both a considerable chapter of public expenditure to be optimized and a lever of economic development to be supported, the Report evaluates the issue of sustainability of the NHS with a medium-term perspective, starting from its primary objective: to promote, maintain and restore people's health.
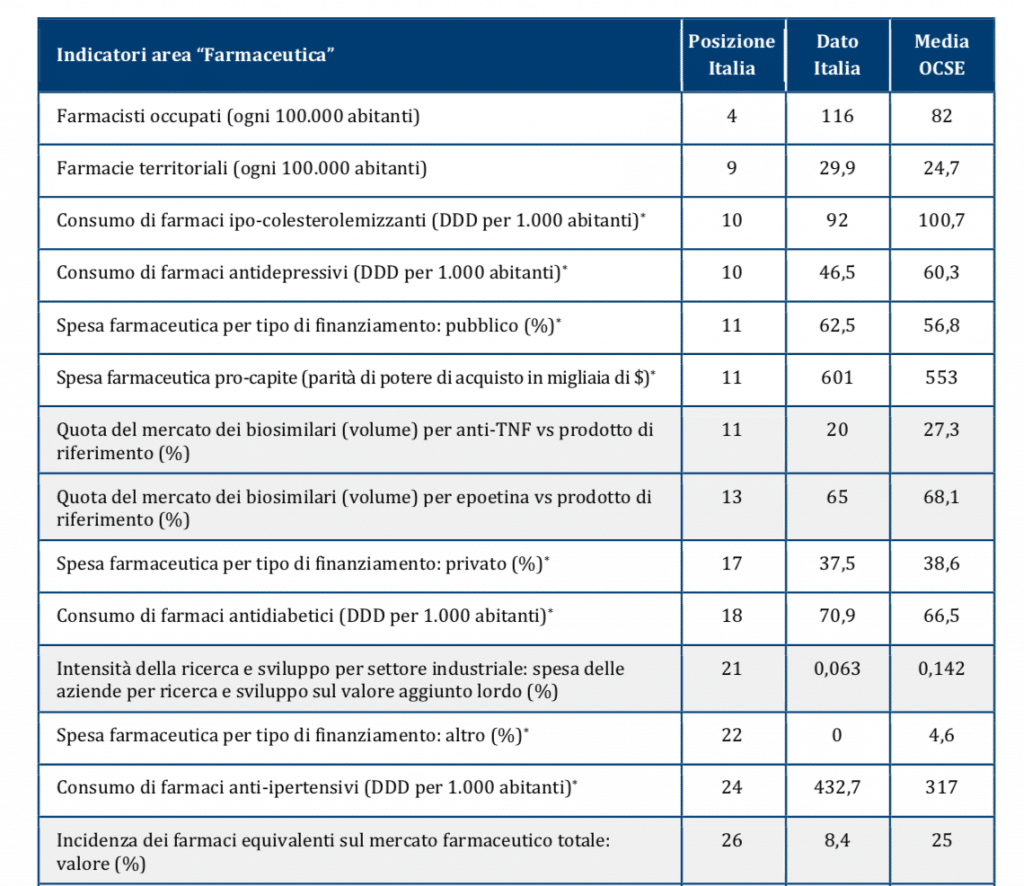
Considering that in the Health at a Glance 2017 report the OECD does not elaborate any rankings, when drafting this Report the GIMBE Foundation analyzed Italy's performance and position for the 76 indicators whose total number after the breakdown is 194.
For each of the 9 performance evaluation categories, a table has been drawn up (tables 1.2-1.10), where for each indicator the position in the ranking of Italy, the national data and the OECD average are reported; the lines highlighted in gray identify the indicators where Italy's performance is worse than the OECD average. In processing the data, Italy's position in the ranking was assigned based on the analysis of the direction of the indicator: when performance improves as the numerical value increases, the ordering is descending; when the performance improves as the numerical value decreases, the sorting is ascending. For the indicators for which the direction cannot be interpreted unequivocally, indicated in the table with an asterisk (*), the ranking has always been drawn up in descending order. At the bottom of each table, the indicators which do not allow for the elaboration of a classification (n.6) and those for which the data relating to Italy is not available (n. 37) are listed; consequently, the total number of indicators included in the tables is 151.